Abstract
Introduction: Since Multiple Myeloma (MM) has seen major advances in the understanding and management of the disease, among them revised disease definitions and recognition of early diagnosis-defining events, early diagnosis and treatment initiation, especially of symptomatic patients (pts), have been advocated by the international and European MM working groups. As a consequence, prompt recognition of MM is essential. However, since MM represents a frequently insidious developing malignancy and may appear with unspecific symptoms, e.g. bone pain or anemia symptoms, this can obscure diagnosis finding and result in substantial delays until the correct diagnosis is made. Objective literature and larger group analyses are lacking and potential risks, which may lead to delayed MM recognition, remain as yet undetermined. This ongoing DSMM project addressed this aspect with the aim to optimize prompt diagnosis finding and to consequently further improve the quality of MM care.
Methods: We performed an initially retrospective analysis in 101 MM pts, followed by a prospective study in 176 pts using a structured MM-specific questionnaire, which was developed within our MM research group, with our comprehensive cancer center and statisticians. The questionnaire consists of 9 items and was initially tested in 10 healthy volunteers in 5 successive rounds, until utmost comprehensibility and perfection were achieved. For both analyses, all available pt medical reports on the duration and type of the initial symptoms leading to the diagnosis of MM were assessed and putative risks for possible delays were determined. The subsequent prospective study was complemented with this questionnaire. This included assessment of pts' satisfaction with the diagnostic process and their suggestions, how it could be improved in the future. The trial protocol and MM-questionnaire were approved by the ethics committee. All pts provided written informed consent and all procedures were conducted in accordance with the Declaration of Helsinki and GCP guidelines.
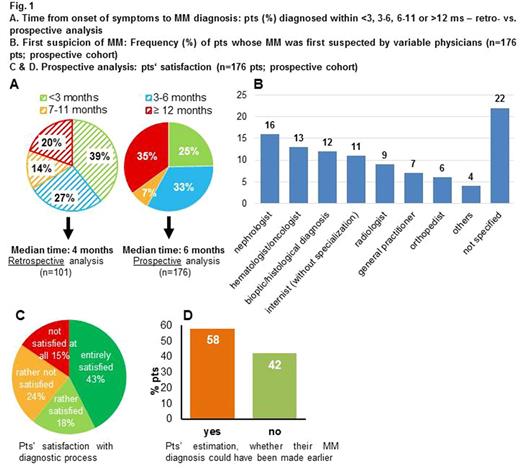
Results: The retro- and prospective MM cohorts showed comparable pt characteristics with typical age and MM features for tertiary centers.The median time from pts' first symptoms to the final MM diagnosis was 4 months (ms; 0.5-120) in the retrospective cohort, and similar in the prospective group with 6 ms (0.5-60). Both analyses showed substantial variations of prompt to much longer latencies (Fig.1A). Of note, 20% in the retrospective analysis and 35% in the prospective study showed a prolonged duration of ≥12ms from symptom onset until the diagnosis of MM was made (Fig.1A). Frequencies of MM-related pathologic bone fractures, renal and infectious complications, occurring before the initial MM diagnosis, were substantial with 41%, 35% and 16%, respectively. 34% of pts had none of these complications at the time of MM diagnosis, 43% had one, 20% two and 3% three complications. Although the most frequent symptom was bone pain, occurring in 73% of MM pts before the final MM diagnosis was made, only 6% of MM diagnoses were first suspected by orthopedists, whereas by nephrologists in 16%, although renal impairment was less frequent (Fig.1B). The final diagnosis of MM was most often made by tertiary centers (81%), followed by outpts' hematologist/oncologist practices (10%) and general practitioners (5%). Of interest, 61% of pts were completely or rather satisfied with the diagnostic process, whereas 39% were less satisfied (Fig.1C). Many more pts than the latter group with 39%, namely 58% of pts, believed that their disease could have been diagnosed more expeditiously (Fig.1D). Those pts, who criticized the longer diagnostic process vs. those that did not, showed a much longer median time interval from symptom onset to their final MM diagnosis of 9 vs. 3 ms. Risks for delays in diagnosis finding were light-chain-only MM, prior orthopedic and rheumatologic comorbidities disguising MM, longer distance to referral centers and pts' residence in smaller rural areas.
Conclusions: Considerable latencies in diagnosis finding of ≥12 ms may occur in MM pts showing unspecific symptoms like bone pain and/or anemia. Longer time intervals from the onset of first symptoms to the MM diagnosis substantially influence pts' coping with their disease and their satisfaction with their MM center. Subsequent analyses aim to generate further insights, how prompt MM diagnosis can be achieved.
Engelhardt: German Cancer Aid (#11424): Other: Educational Grant; Janssen Cilag GmbH: Other: Educational Grant; Celgene GmbH: Other: Educational Grant; Amgen GmbH: Other: Educational Grant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal